Abstract
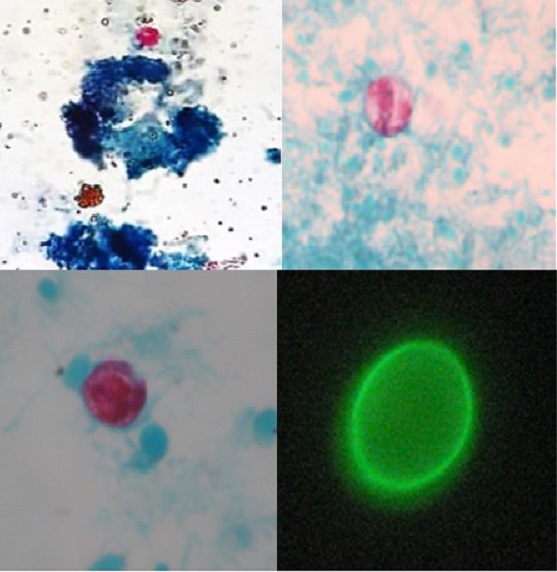
The aim of this study was to investigate an outbreak caused by protozoa, which occurred in a municipality in the Brazil southern region. The investigations were carried out analyzing 47 fresh stool samples and 26 water samples by parasitological and molecular methods, as well as, direct immunofluorescence. After the filtrations of water samples and purification of stool samples, the concentrates were evaluated microscopically for presence of parasites. Molecular analyses were performed by polymerase chain reaction (PCR) for DNA detection of Giardia spp., Cryptosporidium
parvum, C. hominis and Cyclospora cayetanensis. Out of 26 water samples, 30.8% (8/26) had waterborne protozoa and C. cayetanensis was the most prevalent (15.5%). Out of the 47 stool samples, 23.4% (11/47) were infected with
C. cayetanensis and Giardia spp. The results showed that backwash water samples from filters of the Water Treatment Station were contaminated with C. cayetanensis, C. hominis and Giardia spp., suggesting the contamination of water sources with human waste brought by sewage. These results show the importance of protozoa investigation in water and stool samples by laboratory methodologies principally in outbreaks causing acute diarrheal disease.
References
1. Kirk MD, Pires SM, Black RE, Caipo M, Crump JA, Devleesschauwer B et al. World Health Organization Estimates of the Global and Regional Disease Burden of 22 Foodborne Bacterial, Protozoal, and Viral Diseases, 2010: A Data Synthesis. PLoS Med. 2015;12(12):e1001921. https://doi.org/10.1371/journal.pmed.1001921
Erratum in: PLoS Med. 2015;12(12):e1001940. https://doi.org/10.1371/journal.pmed.1001940
2. Bandsma RHJ, Sadiq K, Bhutta ZA. Persistent diarrhoea: current knowledge and novel concepts. Paediatr Int Child Health. 2019;39(1):41-47. https://doi.org/10.1080/20469047.2018.1504412
3. Pires SM, Fischer-Walker CL, Lanata CF, Devleesschauwer B, Hall AJ, Kirk MD et al. Aetiologyspecific estimates of the global and regional incidence and mortality of diarrhoeal diseases commonly transmitted through food. PLoS One. 2015;10(12):e0142927. https://doi.org/10.1371/journal.pone.0142927
4. Ramírez-Castillo FY, Loera-Muro A, Jacques M, Garneau P, Avelar-González FJ, Harel J et al. Waterborne pathogens: detection methods and challenges. Pathogens. 2015; 4(2): 307-34. https://doi.org/10.3390/pathogens4020307
5. Behera B, Mirdha BR, Makharia GK, Bhatnagar S, Dattagupta S, Samantaray JC. Parasites in patients with malabsorption syndrome: a clinical study in children and adults. Dig Dis Sci. 2008;53(3):672-9. https://doi.org/10.1007/s10620-007-9927-9
6. Center Control Diseases – CDC. Detecting and Investigating Waterborne Diseases and Outbreaks [Accessed on 2021 Jun 01]. Available from: https://www.cdc.gov/healthywater/surveillance/detecting-investigating.html
7. Semenza, J.C. Cascading risks of waterborne diseases from climate change. Nat Immunol. 2020;21:484-7. https://doi.org/10.1038/s41590-020-0631-7
8. Almeida JC, Martins FD, Ferreira Neto JM, Santos MM, Garcia JL, Navarro IT et al. Occurrence of Cryptosporidium spp. and Giardia spp. in a public water-treatment system, Paraná, Southern Brazil. Rev Bras Parasitol Vet. 2015;24(3):303-8. https://doi.org/10.1590/S1984-29612015051
9. Nyachuba DG. Foodborne illness: is it on the rise? Nutr Rev. 2010;68(5):257-69. https://doi.org/10.1111/j.1753-4887.2010.00286.x
10. Baldursson S, Karanis P. Waterborne transmission of protozoan parasites: review of worldwide outbreaks – an update 2004-2010. Water Res. 2011;45(20):6603-14. https://doi.org/10.1016/j.watres.2011.10.013
11. Efstratiou A, Ongerth JE, Karanis P. Waterborne transmission of protozoan parasites: review of worldwide outbreaks – an update 2011-2016. Water Res. 2017;114:14-22. https://doi.org/10.1016/j.watres.2017.01.036
12. Ministério da Saúde (BR). Secretaria de Vigilância em Saúde. Coordenação-Geral de Laboratórios de Saúde Pública. Manual de diagnóstico dos agentes oportunistas: parasitos intestinais e Pneumocystis jirovecii. Brasília: Ministério da Saúde; 2012. [Accessed on 2021 Jun 01]. Available from: http://www.ial.sp.gov.br/resources/editorinplace/ial/2016_3_11/manual_oport.pdf
13. Sheather AL. The detection of intestinal protozoa and mange parasites by a floatation technique. J Pathol Therap. 1923;36:266-75
14. Rigo CR, Franco RM. Comparison between the modified Ziehl-Neelsen and Acid-Fast-Trichrome methods for fecal screening of Cryptosporidium parvum and Isospora belli. Rev Soc Bras Med Trop. 2002;35:209-14. https://doi.org/10.1590/s0037-86822002000300002
15. Mahbubani MH, Bej AK, Perlin MH, Schaefer FW 3rd, Jakubowski W, Atlas RM. Differentiation of Giardia duodenalis from other Giardia spp. by using polymerase chain reaction and gene probes. J Clin Microbiol. 1992;30:74-8. https://doi.org/10.1128/jcm.30.1.74-78.1992
16. Cacciò SM, Ryan U. Molecular epidemiology of giardiasis. Mol Biochem Parasitol. 2008;160(2):75-80. https://doi.org/10.1016/j.molbiopara.2008.04.006
17. Marciano MAM. Pesquisa de Giardia spp., Cryptosporidium spp., Toxoplasma gondii e Cyclospora cayetanensis em água para consumo humano. [tese de doutorado]. São Paulo (SP): Universidade de São Paulo; 2019.
18. Jothikumar N, da Silva AJ, Moura I, Qvarnstrom Y, Hill VR. Detection and differentiation of Cryptosporidium hominis and Cryptosporidium parvum by dual TaqMan assays. J Med Microbiol. 2008;57(Pt9):1099-105. https://doi.org/10.1099/jmm.0.2008/001461-0
19. Murphy HR, Lee S, da Silva AJ. Evaluation of an improved U.S. food and drug administration method for the detection of Cyclospora cayetanensis in produce using real-time PCR. J Food Prot. 2017;80(7):1133-44. https://doi.org/10.4315/0362-028X.JFP-16-492
20. Ministério da Saúde (BR). Portaria GM/MS nº 888, de 4 de maio de 2021. Altera o Anexo XX da Portaria de Consolidação GM/MS nº 5, de 28 de setembro de 2017, para dispor sobre os procedimentos de controle e de vigilância da qualidade da água para consumo humano e seu padrão de potabilidade. Diário Oficial da União. Brasília, DF, 07 mai. 2021. Seção 1(85):126-36.
21. Agência Nacional de Águas (BR). Atlas águas: segurança hídrica do abastecimento urbano. Brasília: ANA; 2021. [Accessed on 2021 Jun 01]. Available from: https://portal1.snirh.gov.br/ana/apps/storymaps/stories/1d27ae7adb7f4baeb224d5893cc21730
22. Ministério da Saúde (BR). Secretaria de Vigilância em Saúde. Departamento de Vigilância Epidemiológica. Manual Integrado de vigilância, prevenção e controle de doenças transmitidas por alimentos. Brasília: Editora do Ministério da Saúde; 2010. [Accessed on 2021 Jun 01]. Available from: http://vigilancia.saude.mg.gov.br/index.php/download/manual-integrado-de-vigilancia-prevencao-econtrole-de-doencas-transmitidas-por-alimentos/?wpdmdl=6996
23. Pandey PK, Kass PH, Soupir ML, Biswas S, Singh VP. Contamination of water resources by pathogenic bacteria. AMB Express. 2014; 4:1-16,e51. https://doi.org/10.1186/s13568-014-0051-x
24. Borja PC. Política pública de saneamento básico: uma análise da recente experiência brasileira. Saúde Soc. 2014;23(2):432-47. https://doi.org/10.1590/S0104-12902014000200007
25. Young I, Smith BA, Fazil A. A systematic review and meta-analysis of the effects of extreme weather events and other weather-related variables on Cryptosporidium and Giardia in fresh surface waters. J Water Health. 2015;13(1):1-17. https://doi.org/10.2166/wh.2014.079
26. Franco RM, Rocha-Eberhardt R, Cantusio Neto R. Occurrence of Cryptosporidium oocysts and Giardia cysts in raw water from the Atibaia river, Campinas, Brazil. Rev Inst Med Trop S Paulo. 2001;43(2):109-11. https://doi.org/10.1590/s0036-46652001000200011
27. Fayer R, Morgan U, Upton SJ. Epidemiology of Cryptosporidium: transmission, detection and identification. Int J Parasitol. 2000;30(12-13):1305-22. https://doi.org/10.1016/s0020-7519(00)00135-1
28. Franco RMB. Protozoários de veiculação hídrica: relevância em saúde pública. Rev Panam Infectol. 2007;9(4):36-43.
29. Teixeira JC, Oliveira GS, Viali AM, Muniz SS. Study of the impact of deficiencies of sanitation on public health in Brazil from 2001 to 2009. Eng Sanit Ambient. 2014;19(1) 87-96. https://doi.org/10.1590/S1413-41522014000100010
30. Fryauff DJ, Krippner R, Prodjodipuro P, Ewald C, Kawengian S, Pegelow K et al. Cyclospora cayetanensis among expatriate and indigenous populations of West Java, Indonesia. Emerg Infect Dis. 1999;5(4):585-8. https://doi.org/10.3201/eid0504.990426
31. Zini RM, Santos CC, Almeida IA, Peresi JT, Marques CC. Atuação do laboratório de Saúde Pública na elucidação do surto de diarreia causado por Cyclospora cayetanensis no município de General Salgado, SP. Rev Inst Adolfo Lutz. 2004;63(1):116-21. [Accessed on 2021 Jun 01]. Available from: https://periodicos.saude.sp.gov.br/RIAL/article/view/34819
32. Moura JE, Penaforte C, Kerti R, Daufenbach LZ, Camargo NJ, Trevisan R et al. Surto de doença diarreica aguda por Cyclospora cayetanensis, Antonina, Paraná. Bol Eletr Epidemiol. 2002;3:3-5
33. Atherholt TB, Lechevallier MW, Norton WD, Rosen JS. Effect of rainfall on Giardia and Crypto. J Am Water Works Assoc. 1998;90(9):66-80. https://doi.org/10.1002/j.1551-8833.1998.tb08499.x
34. Fregonesi BM, Sampaio CF, Ragazzi MF, Tonani KA, Segura-Muñoz SI. Cryptosporidium e Giardia: desafios em águas de abastecimento público. Mundo Saúde. 2012; 36(4):602-9.
35. Meirelles MV. Cryptosporidium infection in Brazil: implications for veterinary medicine and public health. Rev Bras Parasitol Vet. 2010;19:197-204. https://doi.org/10.1590/s1984-29612010000400002
36. Júlio C, Sá C, Ferreira I, Martins S, Oleastro M, Angelo H et al. Waterborne transmission of Giardia and Cryptosporidium river beaches in Southern Europe (Portugal). J Water Health. 2012;10:484-96. https://doi.org/10.2166/wh.2012.030
37. Kumar T, Abd Majid MA, Onichandran S, Jaturas N, Andiappan H, Salibay CC et al. Presence of Cryptosporidium parvum and Giardia lamblia in water samples from Southeast Asia: towards an integrated water detection system. Infect Dis Poverty. 2016;5:3. https://doi.org/10.1186/s40249-016-0095-z

This work is licensed under a Creative Commons Attribution 4.0 International License.
Copyright (c) 2022 Instituto Adolfo Lutz Journal