Abstract
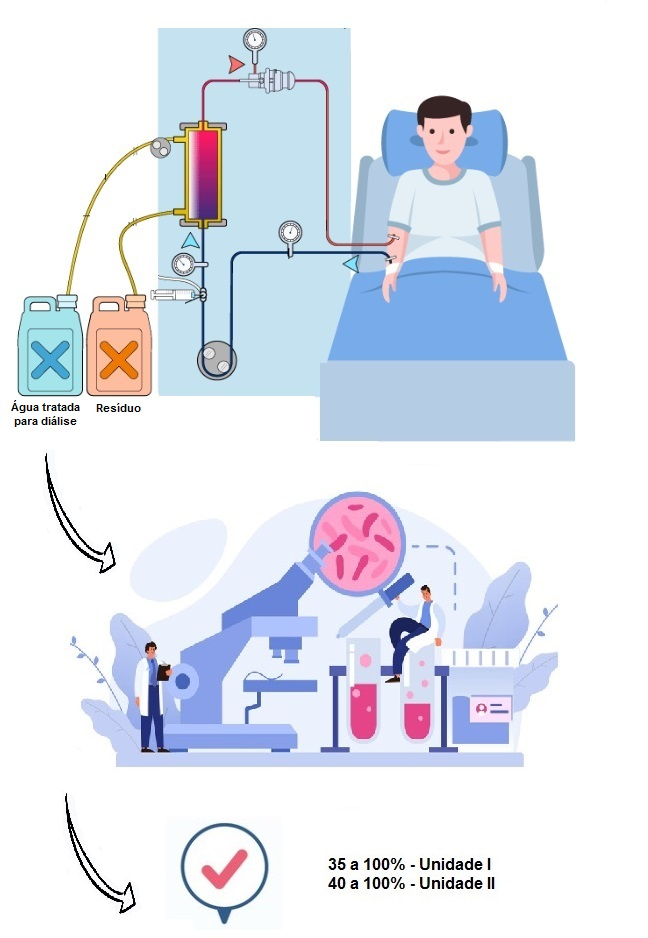
The incidence of acute kidney is high among critically ill patients admitted to Intensive Care Units and is associated with increased mortality, having a major impact on public health. Clinical complications are minimized with dialysis interventions, which expose patients to significant volumes of treated water during in-bed renal therapy. Microbiological analyzes and determination of bacterial endotoxins were performed on treated water samples and dialysate solutions in two public hospitals in São Paulo city, using analytical methodologies recommended in official compendia. The evaluation showed that the percentage of satisfactory results for treated water ranged from 35.2% to 100% in Hospital Unit I and from 40% to 100% in Hospital Unit II between 2010 and 2022. For dialysate solutions in Hospital Unit I, the percentag of satisfactory results was 100% during the same period. The effectiveness of actions implemented by the technical hospital teams, in adapting water for dialysis therapy, points to the importance of encouraging other hospital institutions to standardize and implement a program of continuous improvement for their water treatment systems used in dialysis procedures. This will help to prevent additional risks to patients exposed to renal therapy.
References
1. Menon S, Krallman KA, Arikan AA, Fuhrman DY, Gorga SM, Mottes T et al. Worldwide exploration of renal replacement outcomes collaborative in kidney disease (WE-ROCK). Kidney Int Rep. 2023;8(8):1542-52. https://doi.org/10.1016/j.ekir.2023.05.026
2. Passoni R, Lordani TVA, Peres LAB, Carvalho ARS. Occurrence of acute kidney injury in adult patients hospitalized with COVID-19: A systematic review and meta-analysis. Nefrologia. 2022;42(4):404-14. https://doi.org/10.1016/j.nefro.2021.09.002
3. Meena J, Mathew G, Kumar J, Chanchlani R. Incidence of acute kidney injury in hospitalized children: A meta-analysis. Pediatrics. 2023;151(2):e2022058823. https://doi.org/10.1542/peds.2022-058823
4. Koyner JL, Mackey RH, Rosenthal NA, Carabuena LA, Kampf JP, Echeverri J et al. Health care resource utilization and costs of persistent severe acute kidney injury (PS-AKI) among hospitalized stage 2/3 AKI patients. KIDNEY 360. 2023;360(4):316-25. https://doi.org/10.34067/KID.0005552022
5. Schreider A, Moraes Júnior CS, Fernandes NMS. Three years evaluation of peritoneal dialysis and hemodialysis absorption costing: Perspective of the service provider compared to funds transfers from the public and private healthcare systems. Braz J Nephrol. 2022;44(2):204-14. https://doi.org/10.1590/2175-8239-JBN-2021-0118
6. Pinheiro G, Ruiz PBO, Lima AFC. Custos dos tratamentos destinados a pacientes adultos com Covid-19 em cuidados intensivos: Revisão integrativa. Rev Paul Enferm. 2023;34:a03. https://doi.org/10.33159/25959484.repen.2023v34a03
7. Oliveira IA. Síndrome da lesão renal aguda. Cap 29. In: Moraes Lu, Francescantonio PLC, Pereira MS, Sarkis CM, Taniguchi ALP, organizadores. As bases do diagnóstico sindrômico. Guarujá, SP: Editora Científica Digital Ltda; 2023. 222-7. Disponível em: https://downloads.editoracientifica.com.br/articles/230312429.pdf
8. Zarbock A, Nadim MK, Pickkers P, Gomez H, Bell S, Joannidis M et al. Sepsis-associated acute kidney injury: consensus report of the 28th acute disease quality initiative workgroup. Nature Reviews Nephrology. 2023;19:401-17. https://doi.org/10.1038/s41581-023006833
9. Moreira-Quijije JX, Tigua-Ponce JA, Alcocer-Diaz S. Prevalencia mundial y factores de riesgo de la insuficiencia renal aguda en poblaciones pediátricas. MQRInvestigar. 2023;7(3):323-43. https://doi.org/10.56048/MQR20225.7.3.2023.323-343
10. De Clercq L, Ailliet T, Schaubroeck H, Hoste EAJ. Acute and chronic cardiovascular consequences of acute kidney injury: A systematic review and meta-analysis. Cardiorenal Med. 2023;13(1):26-33. https://doi.org/10.1159/000527198
11. Meena J, Yadav J, Kumar J, Dawman L, Tiewosh K, Mittal A et al. Incidence, predictors, and short-term outcomes of acute kidney injury in children with diabetic ketoacidosis: A systematic review. Pediatric Nephrology. 2023;38:2023-31. https://doi.org/10.1007/s00467-023-05878-1
12. Turgut F, Awad AS, Abdel-Rahman EM. Acute kidney injury: Medical causes and pathogenesis. J Clin Med. 2023;12(1):375. https://doi.org/10.3390/jcm12010375
13. Ethgen O, Murugan R, Echeverri J, Blackowicz M, Harenski K, Ostermann M. Economic analysis of renal replacement therapy modality in acute kidney injury patients with fluid overload. Critical Care Explorations. https://doi.org/10.1097/CCE.0000000000000921
14. Hu X, Yang M, Li X, Chen Y, Ouyang S, Li L. Knowledge, attitude, and practice of nephrologists on the decision for renal replacement therapy. BMC Public Health. 2023;23:654. https://doi.org/10.1186/s12889-023-15530-0
15. Centers for Disease Control Prevention – CDC. Water use in dialysis. [acesso 2023 Jul 21]. Disponível em: https://www.cdc.gov/dialysis/guidelines/water-use.html
16. Saito AK, Wu S. High-grade Staphylococcus lugdunensis bacteremia in a patient on home hemodialysis. Fed Pract. 2023;40(4):1237. https://doi.org/10.12788/fp.0361
17. Tai T, Yamamoto T, Yamaguchi K, Watanabe M, Tanaka H, Muraki Y et al. Evaluation of the meropenem dosage and administration schedule in patients with bacteremia initial therapy. Journal of Infection and Chemotherapy. 2023;29(8):749-53. https://doi.org/10.1016/j.jiac.2023.04.004
18. Hilinski EG, Almodovar AAB, Silva FPL, Pinto TJA, Bugno A. Is dialysis water a safe component for hemodialysis treatment in São Paulo State, Brazil? Braz J Pharm Sci. 2020;56:e17835. https://dx.doi.org/10.1590/s2175-97902019000417835
19. Jesus PR, Ferreira JAB, Carmo JS, Albertino SRG, Vicentini Neto SA, Santos LMG et al. Monitoring the quality of the water used in mobile dialysis services in intensive care units in the city of Rio de Janeiro. Braz J Nephrol. 2022;44(1):32-41. https://doi.org/10.1590/2175-8239-JBN-2020-0217
20. Almodovar AAB, Buzzo ML, Silva FPL, Hilinski EG, Bugno A. Effectiveness of the monitoring program for ensuring the quality of water treated for dialysis in the state of São Paulo. Braz J Nephrol. 2018;40(4):344-50. https://doi.org/10.1590/2175-8239-JBN-2018-0026
21. Ministério da Saúde (BR). Agência Nacional de Vigilância Sanitária. Resolução RDC nº 154, de 15 de junho de 2004. Estabelece o regulamento técnico para o funcionamento dos serviços de diálise. Diário Oficial da União. Brasília, DF, 17 jun 2004. Seção 1(115):65-9.
22. Ministério da Saúde (BR). Agência Nacional de Vigilância Sanitária. Resolução RDC nº 11, de 13 de março de 2014. Dispõe sobre os requisitos de boas práticas de funcionamento para os serviços de diálise e dá outras providências. Diário Oficial da União. Brasília, DF, 14 mar 2014. Seção 1(50):40-2.
23. Instituto Adolfo Lutz. Manual para Orientação – Análise de Água no Instituto Adolfo Lutz. Segunda Revisão, 2012. Disponível em: http://www.ial.sp.gov.br/resources/editorinplace/ial/2016_4_25/manual_de_colheita_de_agua.pdf?attach=true
24. American Public Health Association (US) – APHA. Standard methods for the examination of water and wastewater. 23ª ed. Washington, DC. 2017. ISBN: 978-0-87553-287-5.
25. BRASIL. Agência Nacional de Vigilância Sanitária – ANVISA. Farmacopeia Brasileira. 2019. 6ª ed. v.1. Disponível em: https://www.gov.br/anvisa/pt-br/assuntos/farmacopeia/farmacopeia-brasileira/VOLUME1FB6at2Erratappdfcomcapa.pdf
26. Cesar Neto, JC. A crise hídrica no estado de São Paulo. Geousp – Espaço e Tempo (Online). 2016;19(3):479-84. http://dx.doi.org/10.11606/issn.2179-0892.geousp.2015.101113
27. Marengo JA, Nobre CA, Seluchi ME, Cuartas A, Alves LM, Mendiondo EM et al. A seca e a crise hídrica de 2014-2015 em São Paulo. Revista USP. 2015;106:31-44. https://doi.org/10.11606/issn.2316-9036.v0i106p31-44
28. Soriano E, Londe LR, Di Gregorio LT, Coutinho MP, Santos LBL. Water crisis in São Paulo evaluated under the disaster’s point of view. Ambient Soc. 2016;19:21-42. https://doi.org/10.1590/1809-4422asoc150120r1v1912016
29. Totaro M, Casini B, Valentini P, Miccoli M, Giorgi S, Porretta A et al. Evaluation and control of microbial and chemical contamination in dialysis water plants of Italian nephrology wards. Journal of Hospital Infection. 2017;97:169-74. http://dx.doi.org/10.1016/j.jhin.2017.05.011
30. Parreira AG, Sousa FV, Rocha AP, Souza TM. Monitoramento microbiológico em sistema inovador e sustentável de tratamento de água destinada à hemodiálise. RAHIS. 2017;48-65. https://doi.org/10.21450/rahis.v13i3.3609
31. Gaibor NGT, Sacaluga LG, Ojeda FC, Cotén JRM, Lazo MS. Thermal disinfection in hemodialysis using the A0 concept as dispenser. Nefrologia. 2019;39(5):482-8. https://doi.org/10.1016/j.nefroe.2019.10.006
32. Iorio B, Micco L, Bruzzese D, Nardone L, Russo L, Formisano P et al. Ultrapure dialysis water obtained with additional ultrafilter may reduce inflammation in patients on hemodialysis. J Nephrol. 2017;30:795-801. https://doi.org/10.1007/s40620-017-0422-x
33. Humadat YR, Al-Naseri SK, Abdul-Majeed MA, Jaafar MS, Al-Naemi AN, Najim LA. Membrane filtration enhanced by ultrasound for reducing endotoxin in dialysis water. Desalination and Water Treatment. 2022;272:31-6. https://doi.org/10.5004/dwt.2022.28842
34. Morghad T, Hassaine H, Boutarfi Z, Gaouar S, Bellifa S, Meziani Z. Bacteriological water quality and biofilm formation in the treatment system of the hemodialysis unit in Tlemcen, Algeria. Seminars in Dialysis. 2020;33:394-401. https://doi.org/10.1111/sdi.12898
35. Tawab MEAE, Arafa RAM, Helmy A, Daigham GES. Management of water quality in some dialysis centers between 1 April 2020 and 31 March 2021 in Cairo hospitals, Egypt. The Arab Journal of Scientific Research. 2023;7(7):85-102. https://doi.org/10.21608/ajsr.2023.296409
36. Câmara SAV, Pivetta ANS, Uehara GHM. Pesquisa de endotoxinas em água de hemodiálise. Vigil sanit debate. 2018;6(4):42-6. https://doi.org/10.22239/2317-269x.01158
37. Bolasco P. The production of on-line dialysis water for extracorporeal dialysis: Proposals for na increased safety upgrade: A viewpoint. Journal of Nephrology. 2020;33:405-15. https://doi.org/10.1007/s40620-019-00667-2
38. Shahryari A, Nikaeen M, Hatamzadeh M, Dastjerdi MV, Hassanzadeh A. Evaluation of bacteriological and chemical quality of dialysis water and fluid in Isfahan, Central Iran. Iran J Public Health. 2016;45(5):650-6. Disponível em: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4935709/pdf/IJPH-45-650.pdf
39. Lima BS. Avaliação do desempenho essencial das máquinas de hemodiálise de um EAS de grande porte [trabalho de conclusão de curso]. Uberlândia (MG): Universidade Federal de Uberlândia; 2020. Disponível em: https://repositorio.ufu.br/handle/123456789/29941
40. Gomes AJS. O impacto da gestão da manutenção nos equipamentos de hemodiálise na segurança e qualidade do atendimento do paciente [trabalho de conclusão de curso de pós-graduação do MBA]. Salvador (BA): Serviço Nacional de Aprendizagem Industrial. 2018. Disponível em: http://repositoriosenaiba.fieb.org.br/bitstream/fieb/1403/1/AILTON%20JOS%c3%89%20DE%0SOUZA%20GOMES.pdf

This work is licensed under a Creative Commons Attribution 4.0 International License.
Copyright (c) 1969 Márcia Buzzo, Adriana Almodovar , Ellen Hilinski